We have seen countless patients in our over 30 years experience who suffer from back pain. Not just short-term back pain, but back pain that has challenged the patient for years and decades. These people continue to suffer from back pain while their doctors try to figure out what is wrong with them. Why is it so hard to figure out what is wrong with them? Why have so many treatments, and even possibly surgery, failed them? It should be easy to figure out, shouldn’t it? Back pain must mean bulging, slipping or herniated disc, correct? No it is not always the discs that are causing back pain and that is why we see some patients who go on for years and years with back pain. Someone is always trying to treat the disc problem when the discs are not the pain problem.
But the MRI says it must be a herniated disc that is causing the problem
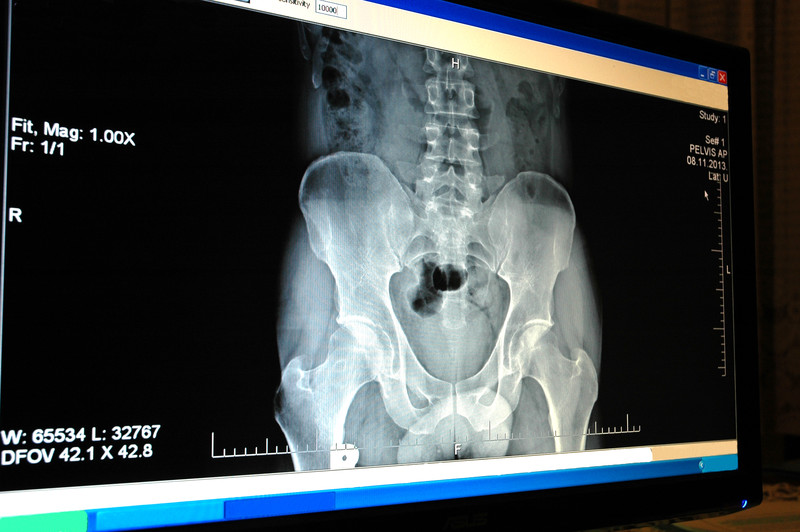
A doctor looking at that MRI would immediately see the herniated disc and possibly suggest that this patient get a discectomy, a surgery to remove the disc and replace it with an artificial disc or a spinal fusion surgery.
Yet there are many structures in the spine that can cause the patient’s pain beyond a herniated disc on an MRI.
Let’s look at the evidence from new and recent medical studies that tell doctors that they have to stop looking at the MRI as the ultimate source of what is hurting the patient.
A report in the Journal of neurosurgery (1) suggests that patients will undergo a surgery, even if they have no pain, if their MRI showed an abnormality.
More than 50% of the 121 patients in the study patients indicated that they would undergo spine surgery based on abnormalities found on MRI, even without symptoms
More than 40% of patients indicated the same for plain radiographs (such as an x-ray).
Similarly, a large proportion of patients (33%) believed that back surgery was more effective than physical therapy in the treatment of back pain without leg pain.
Nearly one-fifth of the survey group (17%) also believed that back injections were riskier than back surgery.
In this study the investigators admitted that they were surprised by the level of misconception regarding the treatment and diagnosis
These results show that a surprisingly high percentage of patients have misconceptions regarding the diagnosis and treatment of lumbar spondylosis (degenerative discs).
Patients overemphasize the value of radiological studies and have mixed perceptions of the relative risk and effectiveness of surgical intervention compared with more conservative management.
These misconceptions have the potential to alter patient expectations and decrease satisfaction, which could negatively impact patient outcomes and subjective valuations of physician performance.
“Patient dissatisfaction with the medical management of low back pain.”
A 2018 study (2) found similar problems. Here researchers found ” common themes” that emerged among the study patients that “highlighted areas of patient dissatisfaction with the medical management of low back pain, in particular, the superficial approach to care perceived by patients and concerns regarding pharmacotherapy. Patients perceive unmet needs from medical services, including the need to obtain a diagnosis (needing to go to too many doctors), the desire for pain control and the preference for spinal imaging. (Patients want an MRI because they believe that will tell them everything).
“Too much imaging”
A 2019 study (3) suggested that people with low back pain are centered around their desire for a diagnosis, potentially contributing to expectations for and overuse of imaging. People with low back pain expressed a strong desire for clear, consistent and personalized information on prognosis, treatment options and self-management strategies, related to healthcare and occupational issues.”
What you just read is something we see all the time in our office. A patient with a lot of images insisting that we treat the herniated disc. After we do a detailed physical examination we explain to the patient, on many occasions, that we do not believe the disc is the cause of their problems but micro tears of the spinal ligaments, muscles, tendons and fasica that is causing their spine to rotate out of position.
But how can the MRI be the wrong path to treatment?
In the medical journal Spine, doctors looked at the top 100 cited medical research papers on back pain. The number one and number two articles tackled the problem of how doctors needed to explain the peculiar problem of why a patient has no symptoms or pain but their MRI suggests extensive spinal abnormalities including herniated discs.(4) Obviously this is a point of great concern for doctors, what to do with an MRI reading that shows something on film but not in the patient. How do you treat the patient?
In 2020, an updated list of the top 100 cited medical research papers on back pain was produced. (5) The top paper in 2020 remained the 1990 “Abnormal Magnetic-Resonance Scans of the Lumbar Spine in Asymptomatic Subjects. A Prospective Investigation.” (6) Thirty years later, doctors are still referring to this paper to figure out why people with really bad MRIs have no back pain.
Confusing diagnosis sends people to back surgery they did not need
As pointed out, there are many things that can cause spinal instability and back pain. The MRI shows a disc problem, but it may not show ligament strain or sprain. It may not show muscle spasms. Soft tissue injury can cause significant pain and instability while the herniated disc causes no pain, but if captured on film – will send the patient off to a surgical recommendation and a date for fusion or other procedure.
If you would like to explore more information, please contact our office so we can start a conversation with you.
Related articles
Epidural Spinal Injections – Will They Help You?
Epidural Spinal Injections – Will They Help You?
Epidural Spinal Injections – Will They Help You?
1 Franz EW, Bentley JN, Yee PP, Chang KW, Kendall-Thomas J, Park P, Yang LJ. Patient misconceptions concerning lumbar spondylosis diagnosis and treatment. J Neurosurg Spine. 2015 May;22(5):496-502. doi: 10.3171/2014.10.SPINE14537. Epub 2015 Feb 27.
2 Chou L, Ranger TA, Peiris W, et al. Patients’ perceived needs for medical services for non-specific low back pain: A systematic scoping review. PLoS One. 2018;13(11):e0204885. Published 2018 Nov 8. doi:10.1371/journal.pone.0204885
3 Lim YZ, Chou L, Au RT, et al. People with low back pain want clear, consistent and personalised information on prognosis, treatment options and self-management strategies: a systematic review. J Physiother. 2019;65(3):124-135. doi:10.1016/j.jphys.2019.05.010
4 Steinberger J, Skovrlj B, Caridi JM, Cho SK. The top 100 classic papers in lumbar spine surgery. Spine 2015 May 15;40(10):740-7. doi: 10.1097/BRS.0000000000000847.
5 Aldawsari K, Alotaibi MT, Alsaleh K. Top 100 Cited Articles on Lumbar Spondylolisthesis: A Bibliographic Analysis. Global Spine J. 2020 May;10(3):353-360. doi: 10.1177/2192568219868194. Epub 2019 Aug 20. PMID: 32313801; PMCID: PMC7160804.
6 Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72(3):403-408.




































Recent Comments