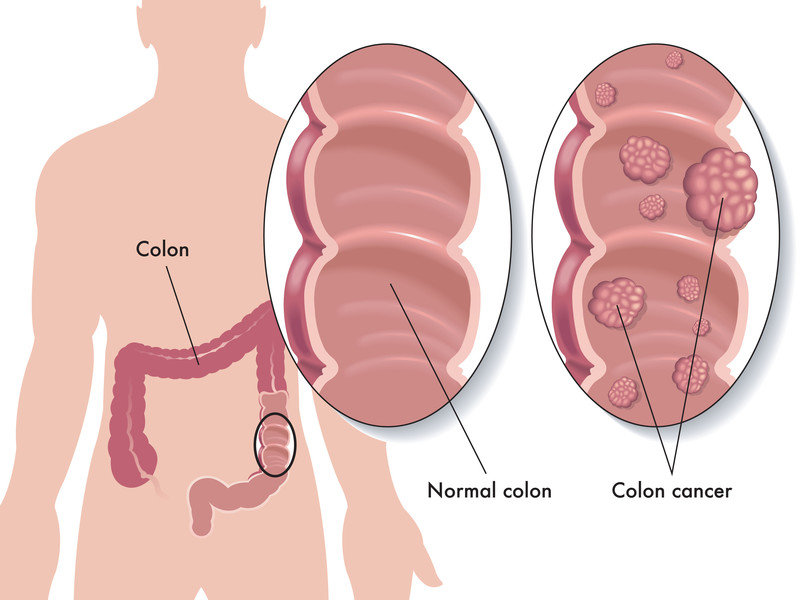
In monitoring the latest science and research findings, we have seen numerous studies addressing the problems and impact of chronic intestinal inflammation and the development of colon cancer. This serious health threat can likely be a preventable one for many people at risk.
In this article we will discuss the well known inflammatory bowel diseases and how they can develop into colon cancer. We will also discuss prevention strategies.
Irritable bowel syndrome
Irritable bowel syndrome, or IBS, is a bowel disorder characterized by abdominal pain and cramping, intestinal gas and bloating, as well as changes in bowel movements without a known reason.
Colitis is an inflammatory bowel disease that results in chronic swelling of the digestive tract, usually in the large intestine (colon) and the rectum. Colitis generally refers to two common types of conditions, either Crohn’s Disease, an autoimmune disease in which the body’s immune system attacks the gastrointestinal tract, or ulcerative colitis, a type of inflammatory bowel disease (IBD) that affects the lining of the large intestine (colon) and rectum. Many patients with these conditions exhibit diarrhea, abdominal pain, bloating, weight loss, and frequent bowel movements.
“Colitis-associated cancer”
A study published in the medical journal Cancer research (1) examined the link between chronic colon inflammation and colon cancer risk. These are the highlight findings of this research.
Inflammation promotes tumor development: The increased risks conferred by inflammatory bowel disease (IBD) to the development of colorectal cancer gave rise to the term “colitis-associated cancer” and the concept that inflammation promotes colon tumorigenesis.
Hidden low grade inflammation can cause development of cancer: A condition more common than IBD is low-grade inflammation, which correlates with altered gut microbiota composition and metabolic syndrome, both present in many cases of colorectal cancer.
Low-grade inflammation caused by artificial food stuffs: Recent findings suggest that low-grade inflammation in the intestine is promoted by consumption of dietary emulsifiers, a ubiquitous component of processed foods, which alter the composition of gut microbiota.
Disruption or stress in the colon can promote cancer development: These findings support the concept that perturbations (stress) in host-microbiota interactions that cause low-grade gut inflammation can promote colon carcinogenesis.
Research: Diet is perhaps the biggest factor that can exert the greatest influence on colorectal cancer risk from inflammation.
The findings of the above study make these key suggestions: High-grade and low-grade inflammation in the colon can cause tumor development. Tumor development is fed by artificial additives, bad bacteria in the gut, and the development of Metabolic Syndrome. Further, these are conditions that can be managed and reversed with proper diet.
Cancer starts in the Pre-Diabetes stage with a Pro-Inflammatory Diet
Doctors at the University of South Carolina examined the role of a pro-inflammatory diet in the risk of cancer mortality. Publishing in the European Journal of Nutrition, (2) these researchers focused on the relationship between diet-associated inflammation, as measured by dietary inflammatory index (DII) score, and mortality, with special focus on prediabetics.
According to its creators, Connecting Health Innovations, “The DII® estimates the inflammatory potential of one’s diet through data provide by having individuals and/or clinicians fill out a food frequency questionnaire. The resulting DII® score is then used to educate and inform individuals about the quality of their diet.”
The researchers used this tool and other tools in following test patients. This is the finding they published on developing diabetes and cancer risk: A pro-inflammatory diet, as indicated by higher DII scores, is associated with an increased risk of all-cause, heart disease, all-cancer, and digestive-tract cancer mortality among prediabetic subjects.
The long inflammatory path from poor diet to colon cancer
To connect some more dots, researchers at the University of Massachusetts Medical School wrote in the medical journal: Current opinion in endocrinology, diabetes, and obesity (3) that Insulin resistance, simply your body’s inability to regulate blood sugar, a requisite precursor for the development of type 2 diabetes mellitus, has been implicated in the development of abdominal obesity. Abdominal obesity has been implicated in creating a whole body inflammatory environment. Abdominal obesity has been linked to colon cancer.
In a November 2018 study, in the European journal of epidemiology (4) doctors focused on the various factors of Metabolic Syndrome and its relationship to colon cancer. Here abdominal obesity becomes a factor. The components of Metabolic Syndrome they looked at were glucose intolerance, abdominal obesity and low HDL-C (good cholesterol) levels.
What they found was if you had all three of these problems you had a higher risk of developing colon cancer. A dominating mechanism in this triple threat, chronic inflammation.
“The Role of Dyslipidemia in Colitis-Associated Colorectal Cancer”
In February 2021,(5) a study published in the Journal of Oncology, with the title, The Role of Dyslipidemia in Colitis-Associated Colorectal Cancer presented the path from dyslipidemia (an elevation of lipids in the blood) to cancer. The path was a path of inflammation.
“Dyslipidemia, characterized by metabolic abnormalities, has become an important participant in colorectal cancer. Dyslipidemia aggravates intestinal inflammation, destroys the protective mucous layer, and disrupts the balance between injury and recovery.”
In the next sentence, the study authors present a paradox that cancer has somehow tricked the body to suit its (cancer) needs. This is the realm of variants and mutations.
“On the other hand, antioxidants induced by oxidative stress enhance glycolysis (the breakdown of glucose) to maintain the acquisition of ATP (Adenosine triphosphate, the molecule that carries energy within cells) allowing epithelial cells (blood vessel and skin cells) with damaged genomes (the genes of the cell) to survive.”
What is happening that the body is responding to oxidative stress by releasing anti-oxidants from glucose to support the energy (ATP) needed to start a repair on damaged cells. Whatch what the cancer does.
“In the repetitive phase of colitis, survival factors enable these epithelial cells to continuously proliferate. The main purpose is to restore and rebuild damaged mucosa, mainly aiming to recover mucosal damage and reconstruct mucosa, but it is also implicated in the occurrence and malignancy of colorectal cancer. . . In response to available fat, tumor cells reprogram their metabolism to better plunder energy-rich lipids and rapidly scavenge these lipids through continuous proliferation. However, lipid metabolic disorders inhibit the function of immune-infiltrating cells in the tumor microenvironment through the cross-talk between tumor cells and immunosuppressive stromal cells, thereby providing opportunities for tumor progress.”
The artificial food inflammatory element on the path to colon cancer
Let’s try here to paint a bigger picture of the role of inflammation and its relationship with artificial food stuffs in the development of colon cancer.
In the research from Georgia State University we cited above, those doctors stated that recent findings suggest that low-grade inflammation in the intestine is promoted by consumption of dietary emulsifiers, a ubiquitous component of processed foods, which alter the composition of gut microbiota.
In another paper this same idea is expressed. Here researchers from Israel wrote (6) in the medical journal Gut microbes:
“Obesity is associated with altered gut microbiota and low-grade inflammation. Both dietary habits and food composition contribute to the onset of such diseases. Emulsifiers, compounds commonly used in a variety of foods, were shown to induce body weight gain, low-grade inflammation and metabolic disorders. These dietary compounds promote gut microbiota alteration and gut barrier dysfunction leading to negative metabolic alterations.”
The keywords here of course are artificial sweeteners, low grade inflammation, weight gain, metabolic disorders. Everything is linked through the inflammatory response.
Guides to colon cancer prevention
In the research above you see that there is a long inflammatory and destructive path towards colon cancer. This path is typically a long journey. In that same light, you need to prepare yourself for the long journey back from inflammation.
Researchers from the German Institute of Human Nutrition Potsdam-Rehbruecke quantified the impact of combined multiple healthy lifestyle behaviors on the risk of developing colorectal cancer. They wrote of the formation of a healthy lifestyle index in the Journal of gastroenterology: (7)
The healthy lifestyle index was composed by the following lifestyle factors:
a healthy weight;
low abdominal fat;
participating in regular physical activity;
not smoking and limiting alcohol;
a diet high in fruits, vegetables, fish, yogurt, nuts and seeds, and foods rich in fiber, and low amounts of red and processed meat.
The researchers found that the more healthy lifestyle factors the subjects adopted, the lower their risk of bowel cancer. Compared to people who had followed up to one healthy lifestyle behavior, those who practiced a combination of two, three, four and all the five healthy behaviors had a 13%, 21%, 34% and 37% lower risk of developing bowel cancer, respectively.
Avoid a carbohydrate-rich diet, which results in high blood glucose and insulin which raises risks of colorectal cancer
Doctors from Italy wrote in the International Journal of Cancer:(8)
A carbohydrate-rich diet, resulting in high blood glucose and insulin, has been hypothesized as involved in developing colorectal cancer
Increasing high glycemic index carbohydrate intake was significantly associated with increasing colorectal cancer risk
Increasing low glycemic index carbohydrate intake was associated with reducing risk
High dietary glycemic index and high glycemic index carbohydrate intake were associated with increased risks of cancer at all colon sites
These findings suggest that high dietary glycemic index and high carbohydrate intake from high glycemic index foods are associated with increased risk of colorectal cancer.
“What can I take?”
When a patient comes into our office with problems of the bowel, intestines and colon, they often ask, “What can I take?” We make recommendations based on research. The research can be voluminous so we will touch on the tip of the iceberg here.
New research suggests the following for colorectal cancer risk reduction:
A March 2018 study in the journal Clinical & translational oncology (9) supports earlier research that using American ginseng as a supplement would help reverse chronic intestinal inflammation and as such reduce the risk factor for colorectal cancer. In an early study doctors at the University of Chicago wrote of American ginseng’s ability to reduce the inflammatory effects on colitis in laboratory animals. Not only did they discuss the reduction of inflammation, but the doctors also discussed that ginseng “significantly promoted recovery from the colitis” (10)
In recent published research gathered from a 15 year study, (11) scientists followed patients at higher risk for recurrent cancers of the large bowel. What they were looking for was the preventive potential of vitamins (A, C and E) and selenium supplementation.
Here is what the scientists did:
A total of 411 patients were randomized to receive either an active compound (200 μg selenium, 30 mg zinc, 2 mg vitamin A, 180 mg vitamin C, 30 mg vitamin E) or a placebo daily for 5 years. Of them, 330 had follow-up colonoscopy (164 in the intervention and 166 in the placebo group).
After an average follow-up of 4 years, 100 patients had a recurrence: 38 in the intervention and 62 in the placebo arm. The 15-year cumulative incidence of recurrence was 48.3 % in the intervention and 64.5 % in the placebo arm.
A 39 % reduction of the risk of recurrence was observed in the intervention compared to the placebo group.
“This study showed study showed a statistically significant effect of antioxidant supplementation on adenoma recurrence.”
The Magaziner Center’s Comprehensive Cancer Support Program
The Magaziner Center’s Comprehensive Cancer Support Program combines conventional, complementary and functional therapies individualized to the needs of each patient. We place great emphasis on an extremely thorough series of lab tests to evaluate the cells of the immune system, inflammatory markers, antioxidant defenses, nutritional status, and overall toxic burden. Most of our patients have already been through the rigors of conventional treatments but have either experienced adverse side effects or unsatisfactory outcomes or both.
Our whole-body approach to cancer includes a variety of therapies, such as nutrition and lifestyle counseling, dietary modifications, supplementation, intravenous vitamin C and other substances, oxidative therapies, immunotherapy, detoxification, lifestyle modifications and exercise therapy, spirituality and mind-body techniques, including stress management and meditation, all with the goal of strengthening the immune system and restoring normal cellular function.
Our treatments are also focused on reducing inflammation, enhancing cellular immune response, improving mitochondrial function, reducing risks of blood clots and inactivating cancer stem cells or cancer initiating cells, that are likely to cause recurrences and metastasis of the disease and are often far more harmful than the actual tumor cells. We strive to change the microenvironment and behavior of the cancer cells by reducing the fuel for these cells and, at the same time, leaving healthy cells alone.
If you would like to explore more information, please contact our office so we can start a conversation with you.
Related articles:
Irritable Bowel Syndrome: Inflammation in the Gut
Targeting and Supporting the Immune System and Gut Microbiota of Cancer Patients
Changing Your Diet May Kill Cancer Cells
The Problem of Antibiotic Overuse, Gut Inflammation, and Elevated Cancer Risk
REFERENCES
1 Viennois E, Merlin D, Gewirtz AT, Chassaing B. Dietary Emulsifier-Induced Low-Grade Inflammation Promotes Colon Carcinogenesis. Cancer Res. 2017 Jan 1;77(1):27-40. doi: 10.1158/0008-5472.CAN-16-1359. Epub 2016 Nov 7.
2 Deng FE. et al. Association between diet-related inflammation, all-cause, all-cancer, and cardiovascular disease mortality, with special focus on prediabetics: findings from NHANES III. Eur J Nutr. 2016 Jan 29. [Epub ahead of print]
3 Hardy OT, Czech MP, Corvera S. What causes the insulin resistance underlying obesity?. Curr Opin Endocrinol Diabetes Obes. 2012;19(2):81-7.
4 Choi YJ, Lee DH, Han KD, Shin CM, Kim N. Abdominal obesity, glucose intolerance and decreased high-density lipoprotein cholesterol as components of the metabolic syndrome are associated with the development of colorectal cancer. European journal of epidemiology. 2018 Nov 1;33(11):1077-85.
5 Chen K, Guo J, Zhang T, Gu J, Li H, Wang J. The Role of Dyslipidemia in Colitis-Associated Colorectal Cancer. Journal of Oncology. 2021 Feb 12;2021.
6 Suez J, Korem T, Zilberman-Schapira G, Segal E, Elinav E. Non-caloric artificial sweeteners and the microbiome: findings and challenges. Gut Microbes. 2015;6(2):149-55.
7. Bonelli L, Puntoni M, Gatteschi B, et al. Antioxidant supplement and long-term reduction of recurrent adenomas of the large bowel. A double-blind randomized trial. J Gastroenterol. 2012 Oct 13. [Epub ahead of print]
8 Sieri S et al. Dietary glycemic index and glycemic load and risk of colorectal cancer: results from the EPIC-Italy study.Int J Cancer. 2014 Nov 18. doi: 10.1002/ijc.29341.
9 Wang CZ, Huang WH, Zhang CF, Wan JY, Wang Y, Yu C, Williams S, He TC, Du W, Musch MW, Chang EB. Role of intestinal microbiome in American ginseng-mediated colon cancer protection in high fat diet-fed AOM/DSS mice. Clinical and Translational Oncology. 2018 Mar 1;20(3):302-12.
10 Yu C et al. American ginseng attenuates azoxymethane/dextran sodium sulfate-induced colon carcinogenesis in mice. J Ginseng Res. 2015 Jan;39(1):14-21. doi: 10.1016/j.jgr.2014.07.001. Epub 2014 Jul 18.
11 Bonelli L, Puntoni M, Gatteschi B, et al. Antioxidant supplement and long-term reduction of recurrent adenomas of the large bowel. A double-blind randomized trial. J Gastroenterol. 2012 Oct 13. [Epub ahead of print]
































Recent Comments