In many articles on our website, we have demonstrated the numerous studies that suggest that not only is chronic inflammation a heart disease risk, but it is also a risk for the development and progression of cancer. In fact, this connection between inflammation and cancer has, and is, spurring an incredible amount of recent research into how lowing inflammatory markers in the blood can reduce cancer risk.
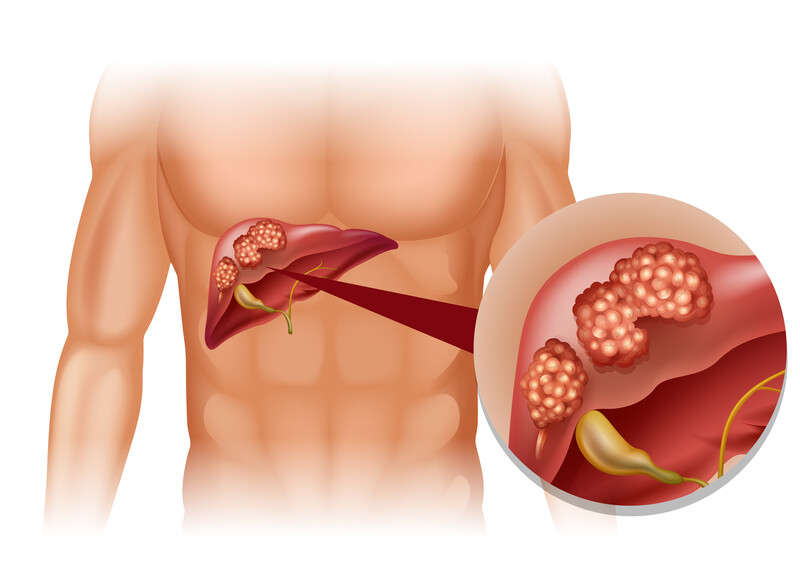
Inflammation and liver cancer
We would like to start this article with a 2014 paper turned book chapter and move our way towards a November 2021 study. This 2014 paper titled: “The role of inflammation and liver cancer,”(1) makes these observations:
“Persistent inflammation is known to promote and exacerbate malignancy. Primary liver cancer, mostly hepatocellular carcinoma (HCC), is a clear example of inflammation-related cancer as more than 90 % of hepatocellular carcinomas arise in the context of hepatic injury and inflammation.
Hepatocellular carcinoma represents the fifth most common malignancy and the third leading cause of cancer-related death worldwide with about one million new cases diagnosed every year with almost an equal number of deaths.
Chronic unresolved inflammation is associated with persistent hepatic injury and concurrent regeneration, leading to sequential development of fibrosis, cirrhosis, and eventually hepatocellular carcinoma.
Irrespective of the intrinsic differences among various etiological factors, a common denominator at the origin of hepatocellular carcinoma is the perpetuation of a wound-healing response activated by parenchymal (liver cells that function, as in cleaning the blood) cell death and the resulting inflammatory cascade.”
Pre-existing liver disorders that lead to cancer
Above you saw the list of pre-existing liver conditions that can turn into cancer because of inflammation. Many liver cancers develop as a result of an underlying liver disease such as hepatitis B or C virus, or non-alcoholic fatty liver disease. Many people with liver disorders also suffer from cirrhosis or scarring of the liver. These disorders lead to increase risk of Hepatocellular carcinoma, as noted above, the most common of primary liver cancers. Research has shown that reducing dietary inflammation may be a way to restore liver health and reduce liver cancer risk.
A well cited and noted 2016 study published in the Annual review of medicine (2) reported:
The burden of hepatocellular carcinoma is steadily growing because obesity, type 2 diabetes, and nonalcoholic fatty liver disease (NAFLD) are replacing viral- and alcohol-related liver disease as major pathogenic promoters. The hepatocellular carcinoma risk connected to metabolic factors has been underestimated so far, and a poorer surveillance has prevented an adequate treatment.
The findings of the above study make these key suggestions: High-grade and low-grade inflammation in the liver can cause tumor development. Tumor development is fed by artificial additives, bad bacteria in the gut, and the development of Metabolic Syndrome, (high cholesterol, type 2 diabetes, high blood pressure). Further, these are conditions that can be managed and reversed with proper diet.
Is diet the only way to reduce chronic inflammation and reduce cancer risk? How about NSAIDs?
In the research there are many ways proposed to lowering inflammation. Recently doctors began exploring the use of Non-steroidal anti-inflammatory medications (NSAIDs) as a preventative cancer treatment. Here is a 2019 paper (3) that explains how these drugs may reduce cancer risk and the drawbacks and side-effect risks of taking these drugs.
“Due to their anti-inflammatory properties, these drugs (NSAIDs) have been investigated for their anticancer effects in numerous studies. This is because chronic inflammation has long been linked to carcinogenesis. As such, anti-inflammatory drugs are believed to play a role in cancer treatment and prevention. In the past few decades, research has shown that NSAIDs may decrease the risk of certain types of cancer. However, there is also a growing body of research that proves the contrary. Furthermore, NSAIDs are well known for many side effects, including some life-threatening ones.”
Because of the related risks with NSAIDs, other researchers took to exploring the idea of reducing inflammation through dietary modification. Diet modification would be safer and a lifestyle change as opposed to medication dosage would be seen as a more successful long-term program.
Inflammatory foods
The purpose of this article is to demonstrate the research and science that suggests dietary modification can reduce liver cancer risk and that a lifestyle modification program would need to be developed beyond the simple inclusion or exclusion of certain foods. Because there a countless articles on the internet that explains which foods are highly pro-inflammatory with varying lists of foods, we will suggest this short and obvious list of foods documented to have carcinogenesis effect and impact on obesity and metabolic syndrome disorders.
Foods with excess sugar.
Foods heavy in refined or processed carbohydrates, such as baked goods.
Fried foods.
Red and processed meats.
Yes there are more foods for this list, this is a simple overview. Now what about the good foods and a good diet plan? Let’s get to the research.
Inflammatory foods and liver cancer
A March 2020 study (4) in the International journal of cancer suggests: “Chronic inflammation plays an important role in primary liver cancer etiology, and can be influenced by dietary habits. Overall, a more pro-inflammatory diet, as suggested by higher DII (Dietary Inflammatory Index) scores, is associated with higher risks of primary liver cancer incidence and mortality. These findings indicate that encouraging intake of more anti-inflammatory dietary components and reducing intake of pro-inflammatory components represent an attractive strategy to reduce primary liver cancer incidence and mortality.”
Magnesium based foods reduce inflammation and risks for primary liver cancer
A February 2020 study (5) also in the International journal of cancer and from the same research group suggests: “. . . findings support that increasing the consumption of foods rich in magnesium may be beneficial in reducing primary liver cancer incidence and mortality.” Leading this group is the dark leafy vegetables.
Change in diet linked to reduced Hepatocellular carcinoma risk
In 2017, noted liver disease researcher Lemonica Koumbi wrote in the World journal of hepatology:(6) “Hepatocellular carcinoma is the third leading cause of cancer mortality. Evidence shows that diet relates to Hepatocellular carcinoma risk and may also have a protective role. Several dietary factors such as vegetables, cereals, fruits, white meat and fish have been found to be inversely associated with Hepatocellular carcinoma risk, whereas a positive correlation has been found with red meat and dietary sugar intakes. The increasing Hepatocellular carcinoma incidence makes its prevention an urgent matter and diet intervention represent an attractive potential.”
A January 2021 (7) study in the journal Nutrients writes: “evidence supports that diet and dietary patterns are relevant factors related to the risk of hepatocellular carcinoma. Certain dietary patterns . . . foods including vegetables, wholegrains, fish, poultry, coffee, macronutrients including monounsaturated fatty acids, and micronutrients including vitamin E, vitamin B9, β-carotene, manganese and potassium may lead to reduced risk of hepatocellular carcinoma.”
Whole grain and dietary fiber intake
Let’s summarize this article here with a November 2021 paper (8) suggesting dietary changes to include whole grains and dietary fiber. This is from the journal Critical reviews in food science and nutrition.
“The relationship between dietary factors and liver disease remains poorly understood. This study evaluated the associations of whole grain and dietary fiber intake with liver cancer risk and chronic liver disease mortality. The National Institutes of Health-American Association of Retired Persons Diet and Health Study cohort recruited 485, 717 retired U.S. participants in 1995-1996. Follow-up through 2011 identified 940 incident liver cancer cases and 993 deaths from chronic liver disease. Compared with the lowest, the highest quintile of whole grain intake was associated with lower liver cancer risk and chronic liver disease mortality in multivariable Cox (a statistical table) models. Dietary fiber was also associated with lower liver cancer risk and chronic liver disease mortality. Fiber from vegetables, beans and grains showed potential protective effect. Here, we show that higher intake of whole grain and dietary fiber are associated with lower risk of liver cancer and liver disease mortality.”
At the Magaziner Center
Diet and reducing chronic inflammation as a means to reduce liver cancer risk has been shown in the research to be effective strategies in treating liver disorders. If you have liver disease or a family history of liver cancer and would like to explore our programs focused on reducing inflammation and enhancing cellular immune response please contact our office so we can start a conversation with you.
Related articles:
Low Testosterone and Depression
Changing Your Diet May Kill Cancer Cells
References
https://drmagaziner.com/cancer/cancer-molds-and-manipulates-your-fat-cells-to-provide-itself-nourishment-and-protection-from-cancer-treatments/
Changing Your Diet May Kill Cancer Cells
References
1 Bishayee, Anupam. “The inflammation and liver cancer.” Inflammation and cancer (2014): 401-435.
2 Marengo A, Rosso C, Bugianesi E. Liver Cancer: Connections with Obesity, Fatty Liver, and Cirrhosis. Annu Rev Med. 2016;67:103–117. doi:10.1146/annurev-med-090514-013832
3 Wong RSY. Role of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) in Cancer Prevention and Cancer Promotion. Adv Pharmacol Sci. 2019 Jan 31;2019:3418975. doi: 10.1155/2019/3418975. PMID: 30838040; PMCID: PMC6374867.
4 Zhong GC, Wang K, Peng Y, et al. Dietary inflammatory index and incidence of and death from primary liver cancer: a prospective study of 103902 American adults [published online ahead of print, 2020 Mar 6]. Int J Cancer. 2020;10.1002/ijc.32954. doi:10.1002/ijc.32954
5 Zhong GC, Peng Y, Wang K, et al. Magnesium intake and primary liver cancer incidence and mortality in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial [published online ahead of print, 2020 Feb 27]. Int J Cancer. 2020;10.1002/ijc.32939. doi:10.1002/ijc.32939
6 Koumbi L. Dietary factors can protect against liver cancer development. World J Hepatol. 2017 Jan 28;9(3):119-125. doi: 10.4254/wjh.v9.i3.119. PMID: 28217247; PMCID: PMC5295144.
7 George ES, Sood S, Broughton A, Cogan G, Hickey M, Chan WS, Sudan S, Nicoll AJ. The Association between Diet and Hepatocellular Carcinoma: A Systematic Review. Nutrients. 2021 Jan 8;13(1):172. doi: 10.3390/nu13010172. PMID: 33430001; PMCID: PMC7826815.
8 Yang Z, Zhou DD, Huang SY, Fang AP, Li HB, Zhu HL. Effects and mechanisms of natural products on Alzheimer’s disease. Critical Reviews in Food Science and Nutrition. 2021 Sep 25:1-21.




































Recent Comments