If you have been suffering with Irritable Bowel Syndrome, you will know that finding relief of your symptoms can be complex, frustrating, and treatment can be very limited in its relief. We see many patients who have followed very strict and demanding diet and nutritional programs only to give up because the effort did not match the results. Simply, it was too much work to get little to no relief.
Irritable Bowel Syndrome can be a difficult challenge for patients. Sometimes the best plans, the greatest of motivations, and the best of desires to get back to wellness can fail because something in the treatment plan is missing. In this article we will look for what can be missing with an eye on chronic inflammation of the bowel.
Probiotics and prebiotics
Research is showing that a healthy gut microbiome can act to prevent inflammation not only in the gut but the body. How does one maintain a healthy gut microbe? A November 2021 paper suggests (1) that it starts with probiotics and prebiotics.
“An estimated 35 million people in the United States and 11.5% of the population globally are affected by IBS. Immunity, genetics, environment, diet, small intestinal bacterial overgrowth (SIBO), and the gut microbiome are all factors that contribute to the onset or triggers of IBS. With strong supporting evidence that the gut microbiome may influence symptoms associated with IBS, elucidating the important microbes (a mixture of probiotics and prebiotics) that contribute to the symptoms and severity is important to make decisions for targeted treatment. As probiotics have become more common in treating IBS symptoms, identifying effective probiotics may help inform future studies and treatment.”
Let’s move onto a March 2021 study (2). We will see what the study authors said and then discuss these findings.
“It has been speculated that diet is a prebiotic for the intestinal microbiota and favors the growth of certain bacteria. (Foods contain prebiotics that help grow beneficial bacteria in the bowel). These bacteria ferment the dietary components, and the products of fermentation act upon intestinal stem cells to influence their differentiation into enteroendocrine cells. (enteroendocrine cells are found in the gastrointestinal tract, stomach and the pancreas. These cells produce gut hormones that are involved in food digestion and absorption.)”
What happens when more bad than good bacteria is produced in the gut?
“The resulting low density (less production) of enteroendocrine cells accompanied by low levels of certain hormones gives rise to intestinal dysmotility, visceral hypersensitivity, and abnormal secretion. This hypothesis is supported by the finding that changing to a low-FODMAP diet (see blow on the FODMAP diet) restores the density of GI cells to the levels in healthy subjects. These changes in gut endocrine cells caused by low-FODMAP diet are also accompanied by improvements in symptoms and the quality of life.” Low-FODMAP is a low carbohydrates, sugar alcohols, and gluten-free diet.
What these researchers suggest is that by changing diet, a person can increase good bacteria in the gut and reduce “fermentation” or bad bacteria in the gut. This is a similar approach to what we do here at the Magaziner Center for Wellness. We look at the impact of diet on the gut microbiota to assess how we may be able to help people who have tried diet modification and other treatments that have failed them. Now let’s see why people di not get good results.
“In general, all of the available treatment options only provide symptom relief for a subset of patients.”
A December 2019 paper (3) from doctors at the University of Leuven in Belgium discusses the traditional treatment strategies for Irritable Bowel Syndrome and why some patients do not see good long-term results.
This is a summary of the researcher’s findings, their work is in italics.
“Irritable bowel syndrome (IBS) is one of the most common functional gastrointestinal disorders encountered in clinical practice. In the absence of an accurate biomarker for the disorder, IBS is mainly diagnosed based symptomology using the Rome criteria.”
The Rome criteria assesses factors that include:
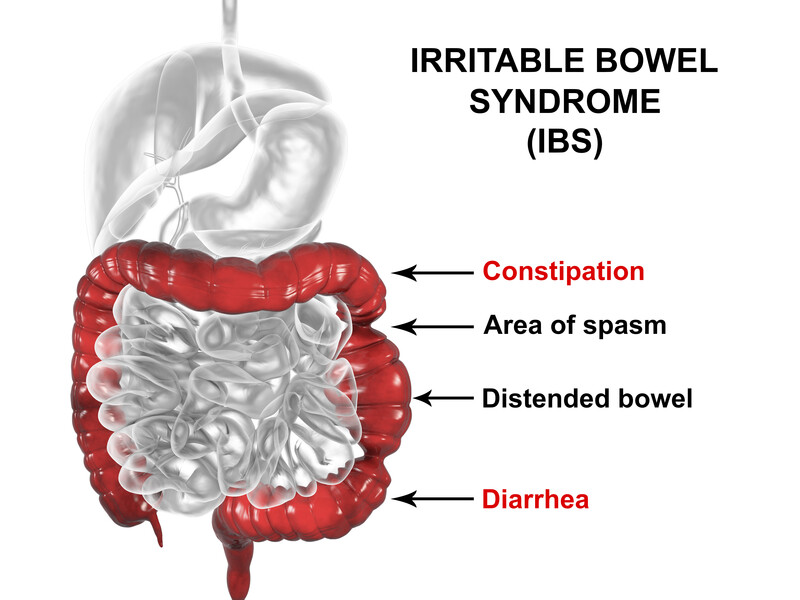
constipation,
diarrhea,
mixed bowel habits,
abdominal bloating/distension,
unspecified functional bowel disorder,and
Opioid-induced constipation.
If you have at least two of these symptoms and abdominal pain and painful bowel movements for at least one day a week, for at least the last three months, that will be the indication that you will get a diagnosis of Irritable Bowel Syndrome. So what do you do about it?
Low-FODMAP – low carbohydrates, sugar alcohols, and gluten-free diet
Citing the research again: “Due to the heterogeneity (the many factors that can cause) this disorder, finding the correct treatment option is often challenging. In general, lifestyle and dietary changes, including the low-FODMAP of gluten-free diet, are the first-in-line treatment for all patients. Issues with dietary changes are the strict elimination of multiple food products and hence difficult compliance to the diet.”
FODMAP is an acronym for “Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.” A group of short chain carbohydrates and sugar alcohols that are poorly absorbed by the body and can cause gastric distress including abdominal pain and bloating. If this diet does not work what can you do?
“When lifestyle changes do not lead to adequate symptom relief, patients should be treated according to their predominant bowel habits and most prominent symptoms. Laxatives or prokinetics and antidiarrheals are used to treat constipation and diarrhea respectively, but have little effect on abdominal pain. To treat GI symptoms, antispasmodics can be attributed.Low doses of neuromodulators (anti-spasmodics) can help gain control over GI and central symptoms, but are also prone to more severe side effects, restricting their widespread use.
Refractory IBS symptoms can be treated with probiotics, antibiotics, histamine-receptor antagonists or alternative therapy, including psychotherapy, hypnotherapy, acupuncture or phytomedicines. However, for many of these options, scientific evidence is sparse and high-quality research is often lacking, leading to inconclusive results.
In general, all of the available treatment options only provide symptom relief for a subset of patients.”
What doctors do not find in standard treatments is what we look for
As we have seen, the diagnosis of Irritable Bowel Syndrome (IBS) is typically based on symptoms, alone, as there is no real test to confirm the condition beyond scans and images that show significant abnormalities in the bowel. At the Magaziner Center for Wellness, we do functional tests versus anatomical tests – we look at how everything functions, rather than just looking at the upper or lower gastrointestinal tract which will typically appear normal in an IBS patient.
Because several conditions may present as IBS, including celiac disease, fructose malabsorption, mild infections, parasitic infections and several inflammatory bowel diseases, we look at food sensitivities, especially to dairy, wheat, corn and soy which are the most common. If a sensitivity or allergy is uncovered, we work with our patients to make necessary modifications to eliminate the trigger from his/her diet. We also look at the problems of inflammation.
Overall, we help move all patients away from an inflammatory diet – one that may include fried foods, sugary carbohydrates, processed foods and artificial sweeteners – to a “Mediterranean” diet centered on healthy fats, lean proteins, fruits and vegetables. We also help patients eliminate the use of medications that may cause bowel inflammation. This is important because repeated use of antibiotics can cause an imbalance of intestinal bacteria (also known as dysbiosis) and some, such as Naproxen, have been linked to the occurrence of “Leaky Gut Syndrome,” which is characterized by damage to the intestinal lining.
To determine if dysbiosis exists, we look at stool samples and the general health of the gastrointestinal tract. The stool tests also allow us to look at fatty acid metabolism, digestion and assimilation (absorption) and the specific bacteria that may be absent or present. When necessary, we utilize enzymes or probiotics to improve metabolism and overall intestinal health.
Some IBS “friendly” diets caused more harm than good – when Irritable Bowel Syndrome advances to Inflammatory Bowel Disease
There is much by way of conflicting evidence of what type of diet will help a patient. Many patients who visit us will tell us about the many diets and self-management plans they have tried, that seemed like a good plan, yet in the end, some IBS ‘friendly,” diets caused more harm than good. Listen to this study from January 2020 (4) which examines failed treatments that can take a patient from Irritable Bowel Syndrome to Inflammatory Bowel Disease.
“Diet represents a crucially important and intuitively relevant topic for Inflammatory Bowel Disease patients. Although a substantial number of patients are prone to follow dietary advice from a variety of sources, including the lay press, there is intriguingly little scientific evidence for such an incitement. This may result in physicians being insufficiently informed about various aspects of nutrition, precluding adequate guidance of their patients with IBD.
Importantly, IBD patients are at risk to develop deficiencies in iron, vitamin B12, folic acid, and several micronutrients, which may even be more pronounced in patients with active disease and those following a restrictive diet.
A western diet with an imbalance between omega-6 (n-6)/omega-3 (n-3) polyunsaturated fatty acids (PUFAs), in favor of n-6 PUFAs, may increase the risk of IBD, whereas a diet high in fruits and vegetables may decrease the risk of IBD. Many approaches to influence the course of IBD with dietary intervention exist. However, to induce or maintain remission in IBD with a change of diet is still in its infancy, and more dietary research is needed before we can apply it in daily practice. Patients with IBD, even in remission, have to be screened regularly for malnutrition.”
What we see is the typically advances of a syndrome to a disease because doctors and patient are not given the adequate tools to manage this problem.
Women with Irritable Bowel Disease – the problems are many including weight concerns
The concerns of how Irritable Bowel Syndrome impacts women stems from the fact that women are twice as likely than men to be diagnosed with the disease.
A May 2020 (5) study sought to compare the profile of body adiposity (body fat), life habits, and the quality of life of women with Irritable Bowel Syndrome with a healthy control group.
This is a case-control study on 70 women, 34 with irritable bowel syndrome and 36 healthy. Quality of Life was assessed, Body adiposity was assessed from body mass index, waist circumference, and waist-to-hip ratio.
Women were asked about gastrointestinal symptoms with food deemed as problematic for carriers of Irritable Bowel Syndrome and the presence of typical comorbidities.
Assessment of life habits included: practice of physical activities, alcoholism, smoking, daytime sleepiness, and exclusion of foods from the feeding routine.
Results:
There was higher volume of central and general adiposity in the case group compared with the control group.
Cases presented a higher chance of developing IBS-related comorbidities.
About of 80% of patients with Irritable Bowel Syndrome have excluded some food but they list 7 to 21 as problematic.
“Compared to the control group, women with irritable bowel syndrome showed greater body adiposity, higher frequency of comorbidities, greater restriction on the consumption of problematic foods and worse quality of life.”
If you are a woman with Irritable Bowel Syndrome and you read this, you may be saying to yourself, tell me something I do not know. Hopefully we can.
The many types of bowel inflammation
As we mentioned at the start of this article, treating chronic inflammation of the bowel and the body as a whole is an important factor in the management of Irritable Bowel Syndrome and indeed Inflammatory Bowel Diseases. This type of inflammation is tricky to understand as it is it not one inflammation type, but could be many inflammation types, all with their unique ways of causing bowel inflammation. This is pointed out by another 2020 study. (6)
“Inflammatory mechanisms of ulcerative colitis and irritable bowel syndrome may overlap or are part of different spectrums. However, potential links between inflammation and IBS-like symptoms in these patient groups are still unclear. . . systemic inflammatory protein profiles distinguish ulcerative colitis patients from irritable bowel syndrome patients, irrespective of inflammation or IBS-like symptoms, suggesting that inflammatory mechanisms of the diseases are part of different spectrums.”
In other words, inflammation is multi-faceted and a more comprehensive approach to treatment including the management of inflammation will be needed for many patients.
This was also suggested by a January 2021 study (7) that suggested: “It is important to re-highlight here that the gut microbes work in consort and therefore, it is not just one microbe species performing these fermentative processes in isolation; this adds to the complexity of the gut environment.” This study focused on pediatric problems.
At the Magaziner Center, we believe in treating the digestive imbalances at the source. Through specialized blood and stool testing, we often find abnormal digestion or assimilation, imbalance in the flora or fatty acid metabolism and leaky gut syndrome or increased intestinal permeability that is triggering problems. Once these imbalances are addressed, we see can see tremendous healing and improvement in our patients.
Using an extremely thorough series of tests, we also look for triggers such as food allergy or intolerance, insufficiencies in nutrients, cellular imbalance, heavy metal excess, imbalance in gastroesophageal bacteria and yeast, and more. We are then able to treat each cause using methods such as nutritional supplementation, sublingual desensitization, and more.
Each of these therapies aim to correct the imbalance or problem, rather than simply suppressing it, improving the overall health and well being of our patients, please contact our office so we can start a conversation with you.
Related articles
Celiac Disease
References
1 Phan J, Nair D, Jain S, Montagne T, Flores DV, Nguyen A, Dietsche S, Gombar S, Cotter P. Alterations in Gut Microbiome Composition and Function in Irritable Bowel Syndrome and Increased Probiotic Abundance with Daily Supplementation. mSystems. 2021 Nov 2:e0121521. doi: 10.1128/mSystems.01215-21. Epub ahead of print. PMID: 34726487.
2 El-Salhy M, Patcharatrakul T, Gonlachanvit S. The role of diet in the pathophysiology and management of irritable bowel syndrome. Indian Journal of Gastroenterology. 2021 Mar 5:1-9.
3 Y. Y. Loong et al. A Review on the Effects of Probiotics and Antibiotics towards Clostridium difficile Infections. Pertanika Journal of Science and Technology, 21 (2): 293 – 302 (2013)
4 Schreiner P, Martinho-Grueber M, Studerus D, Vavricka SR, Tilg H, Biedermann L. Nutrition in Inflammatory Bowel Disease [published online ahead of print, 2020 Jan 10]. Digestion. 2020;1–16. doi:10.1159/000505368
5 Mendonça APM, Yamashita LM, Silva ED, Solar I, Santos LAO, Vasques ACJ. NUTRITIONAL STATUS, QUALITY OF LIFE AND LIFE HABITS OF WOMEN WITH IRRITABLE BOWEL SYNDROME: A CASE-CONTROL STUDY [published online ahead of print, 2020 May 20]. Arq Gastroenterol. 2020;S0004-28032020005004201. doi:10.1590/s0004-2803.202000000-22
6 Moraes L, Magnusson MK, Mavroudis G, et al. Systemic Inflammatory Protein Profiles Distinguish Irritable Bowel Syndrome (IBS) and Ulcerative Colitis, Irrespective of Inflammation or IBS-Like Symptoms [published online ahead of print, 2020 Jan 4]. Inflamm Bowel Dis. 2020;izz322. doi:10.1093/ibd/izz322
7 Armstrong H, Mander I, Zhang Z, Armstrong D, Wine E. Not All Fibers Are Born Equal; Variable Response to Dietary Fiber Subtypes in IBD. Frontiers in Pediatrics. 2021 Jan 15;8:924.




































Recent Comments