In this article we will explore possible benefits of antioxidants on the inflammatory factors that may lead to progression of Macular Degeneration.
In 2019, doctors wrote in the journal Antioxidants (1) : “The risk of macular degeneration can be reduced through the consumption of antioxidant-rich foods, supplements, and nutraceutical formulas. . . Antioxidants including anthocyanins (nutrients in foods that are especially red, purple and blue in color), carotenoids, flavonoids, and vitamins have been shown to reduce the risk of eye-related diseases. Anthocyanins extracted from berries are powerful antioxidants. . . β-Carotene, as well as xanthophyll lutein (spinach and squash for example) and zeaxanthin (spinach, pistachios, egg yokes, for example), have been reported to reduce the risk of macular degeneration.
Flavonoids from plants help in the prevention of eye-related diseases through anti-inflammatory mechanisms. A combination of these antioxidants, vitamins, and minerals possess a synergistic effect on the prevention or risk reduction of macular degeneration.”
Treatment of age-related macular degeneration focuses on antioxidant agents and anti-vascular endothelial growth factor compounds
In December 2020 in the journal Neural regeneration research (2) researchers wrote: “The retina may suffer neurodegenerative damages, as other tissues of the central nervous system do, and serious eye diseases may develop. One of them is age-related macular degeneration, which causes progressive loss of vision due to retina degeneration. Treatment of age-related macular degeneration focuses on antioxidant agents and anti-vascular endothelial growth factor compounds (compounds which promote the growth of new blood vessels in eyes where blood flow may be restricted), among others, that prevent/diminish oxidative stress and reduce neovascularisation respectively. The phytochemicals, medicinal plants and/or plant-diet supplements might be a useful adjunct in prevention or treatment of age-related macular degeneration owing to their antioxidant and anti-vascular endothelial growth factor properties.”
Diet and nutrition may migrate Age-Related Macular Degeneration
This is what Dr. John G. Lawrenson of the University of London and Dr. Laura E. Downie of the University of Melbourne wrote in the medical journal Nutrients, September 2019 (3) in assessing the role of diet and supplementation in combating vision problems in the aging population. His paper is titled: “Nutrition and Eye Health.”
“Acquired vision loss associated with these conditions (Age-Related Macular Degeneration) can be devastating to the individual through its detrimental impact on quality of life, and also impart substantial societal burden. Although the pathogenesis (the origins) of these conditions is not fully understood, there is increasing evidence that their impact can, to some extent, be mitigated by targeting modifiable risk factors. Since diet and nutrition have been linked with the most common diseases affecting the elderly, dietary modification and nutritional supplementation for the prevention and treatment of these diseases has attracted a considerable amount of scientific attention.”
“There is a clear role of inflammation in the pathophysiology of this disease”
One aspect of diet and nutrition’s lifestyle modification factors in Age-Related Macular Degeneration is that they act as anti-inflammatories
In November 2018, a team of medical university researchers in Italy published their findings in the journal Nutrients (4) on the role of inflammation and oxidation in the progression of age-related macular degeneration. One potential approach, they write, to reduce the risk of age-related macular degeneration is the prescription of vitamins and other anti-oxidative micronutrients. The main reason for this choice resides in the theory that macular degeneration can be managed with an anti-inflammatory and anti-oxidant health program. Although the precise causes of age-related macular degeneration remain unknown, there is a clear role of inflammation in the pathophysiology of this disease.
“Gut-retina axis”
Further, they contend, doctors should explore the role of high-fat and high simple-sugar diets on the development of age-related macular degeneration through damage of the gut microbiota that leads to systemic low-grade inflammation. Furthermore, recent evidence indicates a robust interaction between the gut microbiota and retina that is referred to as the “gut-retina axis”. A better understanding of the mechanisms that underlie this connection may help clinicians to prompt new models of personalized care of age-related macular degeneration based on the promotion of healthy nutritional habits and adequate micronutrient intake. These practices could modulate the gut microbiota toward a reduction of dysbiosis, leaky gut and lower gastro-intestinal distress and, consequently, retinal damage.
This research suggested benefits of Vitamin C, vitamin E, Zinc, Carotenoids, the pigments responsible for the yellow, orange, and red colors of many fruits and vegetables, and Beta-Carotene
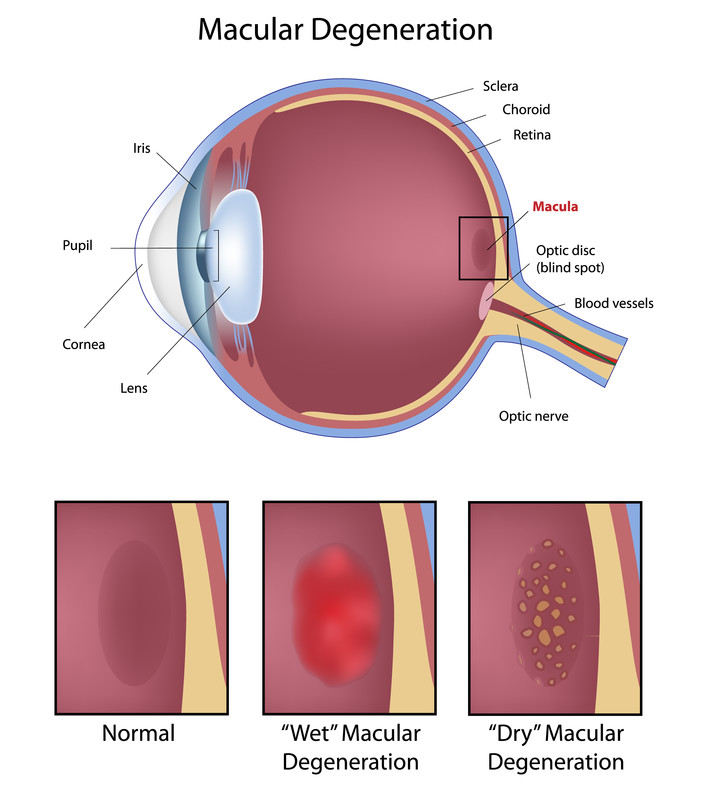
Macular degeneration is characterized by the deterioration of the macula, a small part of the central retina where the eye’s photoreceptors (rods and cones) are most highly concentrated. The leading cause of legal blindness, macular degeneration affects more than 10 million Americans — more than cataracts and glaucoma combined — according to the American Macular Degeneration Foundation. The disease affects a person’s central vision, which is needed for common tasks such as reading and driving. The effect is similar to that of a raindrop on the center of a camera lens.
The role of Vitamin D
In 2017, an international team of scientists published their findings also in the journal Nutrients.(5) Here they write that vitamin D can control the expression of genes involved in oxidative stress, inflammation, and angiogenesis (the formation of new blood vessels that can carry inflammatory factors). In the macula, vitamin D may preserve the function of the retina. Further, they suggest, there is an association between vitamin D deficiency and a higher risk of early and/or late age-related macular degeneration.
This research was followed by a September 2019 study in the medical publication Antioxidants (6) which suggested: “Vitamin D can possibly protect the retina and retinal pigment epithelium (the protective cell layer of the retina) from oxidative stress, inflammation and apoptosis (cell death) through the suppression of pro-inflammatory mediators and by enhancing the antioxidant defence capacity.”
Researchers at the University at Buffalo (7) recently discovered that vitamin D may play a significant role in eye health, specifically in the possible prevention of age-related macular degeneration among women who are more genetically prone to developing the sight-damaging disease.In a paper published in JAMA Ophthalmology online, the University at Buffalo researchers found that women who are deficient in vitamin D and have a specific high-risk genotype (a specific part of their DNA) are 6.7 times more likely to develop age-related macular degeneration than women with sufficient vitamin D status and no high risk genotype. The vitamin D supplementation being a key factor in both groups of women.
Melatonin for Macular Degeneration
In recent years scientists and doctors have made a connection between various characteristics of melatonin, a hormone that regulates the sleep–wake cycle. A 2019 study (8) from the University of Pittsburgh suggests:
“The association between age-related macular degeneration and biological rhythms (sleep–wake cycle) has been insufficiently studied; however there are several reasons to believe that impairment in circadian rhythm (the the natural 24 hour cycle that regulates the sleep-wake cycle) may affect incidence and pathogenesis (onset) of age-related macular degeneration.
The current understanding of age-related macular degeneration pathology is based on age-related, cumulative oxidative damage to the retinal pigmented epithelium partially due to impaired clearance of phagocytosed photoreceptor outer segments. (Note added: The terminology that people with macular degeneration understand are: “rods”, “cones”, and “photosensitive retinal ganglion cells.” These structures gat a daily cleaning or shedding of their outer segments to make way for new cells.)
Every morning, photoreceptor outer segments in the retina are shed, phagocytosed by the retinal pigment epithelium, and degraded to enable renewal. Defects in this process contribute to retinal degeneration. . . Phagocytosis of the outer segments is synchronized by circadian rhythms and occurs shortly after dawn, followed by lysosomal-mediated clearance (simply waste removal). Aging has been shown to be associated with the changes in circadian rhythmicity of melatonin production, which can be a major factor contributing to the impaired balance between phagocytosis and clearance and increased levels of reactive oxygen species resulting in degenerative changes in the retina.”
“Decline with age of the content of melatonin is considered as one of the leading mechanisms of aging and development of associated diseases, including age-related macular degeneration.”
Much of these findings were built on earlier research exploring the same paths.These earlier studies provide a basis for cellular repair with Melatonin.
In a study from 2013 (9) researchers suggested that: “Decline with age of the content of melatonin is considered as one of the leading mechanisms of aging and development of associated diseases, including age-related macular degeneration – the disease, which becomes the most common cause of blindness and acuity of vision deterioration in elderly. The prospects of the use of melatonin in the prevention of age-related macular degeneration is being actively discussed, but as a rule on the basis of the results of the experiments on cells in retinal pigment epithelium. . . Ophthalmoscopic examinations show that Melatonin supplementation decreased the incidence and severity of retinopathy and improved some (but not all) histological abnormalities associated with retinopathy. Thus, melatonin prevented the structural and functional changes in retinal pigment epithelium cells, reduced the severity of microcirculatory disorders. Importantly, Melatonin prevented destruction of neurosensory cells, associative and gangliolar neurons in the retina. Taken together, our data suggest the therapeutic potential of Melatonin for treatment and prevention of age-related macular degeneration.”
Antioxidants for Macular Degeneration
In other research, a study reported in the journal Molecular Vision (10) suggested that zinc oxide combined with a detergent extract of rosemary powder or rosemary oil was found effective in treating eye damage related to age related macular degeneration.
A combined team of Canadian and Pakistani researchers also suggest that Phytonutrients such as lycopene, lutein, and zeaxanthin are particularly helpful in retarding macular degeneration. This study was published in the journal Nutrients.(11)
The third published study we cited above, the researchers also made suggestion that nutrition and supplementation, as demonstrated by research, may not help not help certain individuals. Research is not in agreement. They were able to not one study as follows:
“However, one large, multi-centre Random Controlled Trial conducted in the USA, the Age-Related Eye Disease Study (AREDS), randomized 3640 individuals with AMD to take supplement formulations containing combinations of vitamin C, E, beta-carotene, zinc, and copper, or a placebo, each day.
A major conclusion from the AREDS was that daily, long-term supplementation with vitamin C (500 mg), vitamin E (400 international units (IU)), beta-carotene (15 mg), zinc (80 mg, as zinc oxide), and copper (2 mg, as cupric oxide) reduced the relative risk of progression to late-stage AMD from 28% (observed with placebo) to 20% at 5 years, in people with at least intermediate age related macular degeneration. This means that for people with intermediate age related macular degeneration, who are at the highest risk of progression to late age related macular degeneration, 80 fewer cases would progress for every 1000 people taking the supplement. However, safety concerns were raised regarding high-dose supplementation of the carotenoid used in the original AREDS supplement, beta-carotene, in people who smoke.”(3)
The above research offers suggestions. They should not be followed on a self-help basis. Always consult with your physician before exploring any changes in your daily health routines. If you would like to explore more information, please contact our office so we can start a conversation with you.
References
1 Khoo HE, Ng HS, Yap WS, Goh HJ, Yim HS. Nutrients for prevention of macular degeneration and eye-related diseases. Antioxidants. 2019 Apr;8(4):85.
2 Bosch-Morell F, Villagrasa V, Ortega T, Acero N, Muñoz-Mingarro D, González-Rosende ME, Castillo E, Sanahuja MA, Soriano P, Martínez-Solís I. Medicinal plants and natural products as neuroprotective agents in age-related macular degeneration. Neural regeneration research. 2020 Dec;15(12):2207.
3 Lawrenson JG, Downie LE. Nutrition and Eye Health. Nutrients. 2019 Sep 6;11(9):2123. doi: 10.3390/nu11092123. PMID: 31489894; PMCID: PMC6771137.
4 Rinninella E, Mele MC, Merendino N, et al. The Role of Diet, Micronutrients and the Gut Microbiota in Age-Related Macular Degeneration: New Perspectives from the Gut⁻Retina Axis. Nutrients. 2018;10(11):1677. Published 2018 Nov 5. doi:10.3390/nu10111677.
5 Layana AG, Minnella AM, Garhöfer G, et al. Vitamin D and Age-Related Macular Degeneration. Nutrients. 2017;9(10):1120. Published 2017 Oct 13. doi:10.3390/nu9101120
6 Tohari AM, Alhasani RH, Biswas L, Patnaik SR, Reilly J, Zeng Z, Shu X. Vitamin D Attenuates Oxidative Damage and Inflammation in Retinal Pigment Epithelial Cells. Antioxidants (Basel). 2019 Aug 24;8(9):341. doi: 10.3390/antiox8090341. PMID: 31450606; PMCID: PMC6770403.
7 Millen AE, Meyers KJ, Liu Z, et al. Association between vitamin D status and age-related macular degeneration by genetic risk. JAMA Ophthalmol. 2015;133(10):1171-9.
8 Stepicheva NA, Weiss J, Shang P, Yazdankhah M, Ghosh S, Bhutto IA, Hose S, Zigler JS, Sinha D. Melatonin as the Possible Link Between Age-Related Retinal Regeneration and the Disrupted Circadian Rhythm in Elderly. InRetinal Degenerative Diseases 2019 (pp. 45-49). Springer, Cham.
9 Stefanova NA, Zhdankina AA, Fursova AZh, Kolosova NG. [Potential of melatonin for prevention of age-related macular degeneration: experimental study]. Adv Gerontol. 2013;26(1):122
10 Organisciak DT, Darrow RM, Rapp CM, Smuts JP, Armstrong DW, Lang JC. Prevention of retinal light damage by zinc oxide combined with rosemary extract. Mol Vis. 2013;19:1433-45. Published 2013 Jun 27.
11 Abdel-Aal el-SM, Akhtar H, Zaheer K, Ali R. Dietary sources of lutein and zeaxanthin carotenoids and their role in eye health. Nutrients. 2013 Apr 9;5(4):1169-85. doi: 10.3390/nu5041169. PMID: 23571649; PMCID: PMC3705341.




































Recent Comments