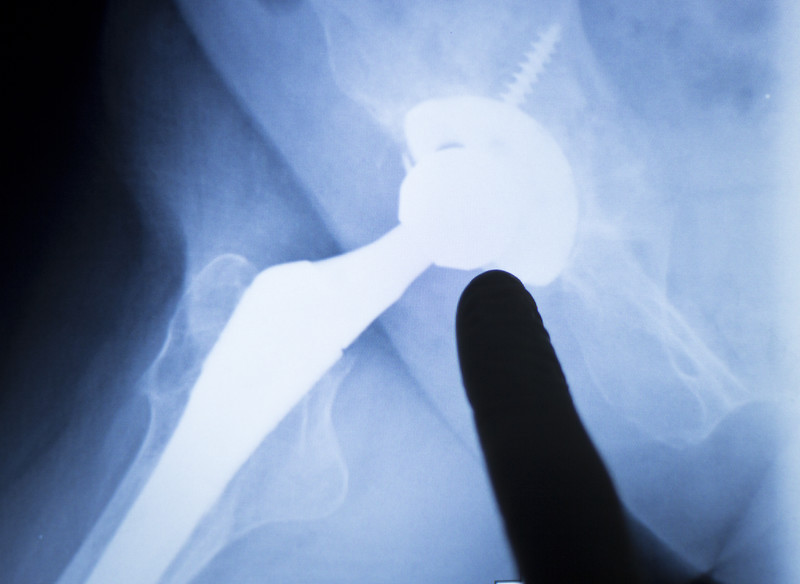
Problems with joint replacement loosening can be much more than a hardware issue. In this article we will look at the role of low hormones in joint replacement loosening problems, and how hormone replacement therapy may help prevent a woman from needing a repair or second total knee or total hip replacement.
We often see post-menopausal women in our office who already had a hip replacement or a knee replacement. They are in our office looking for help because their knee or their hip is very unstable. How did their replacement joint get this way?
Even after a successful joint replacement problems can occur months or years later.
Wear and tear can cause bone loss and a loosening of the prosthetic.
Wear and tear can cause a significant weakening of the structural ligaments and tendons of the hip or knee. The tissue becomes too weak to support the knee or hip replacement and the patient losses stability. Her knee or hip will “give way,” and she can become a “fall risk.”
Weakened bone can cause the formation of bone spurs to stabilize the knee. This will lead to stiffness and loss of range of motion. To prevent your hip or knee from “giving way,” the bone spurs will “lock things up,” and prevent excessive movement.
As you can see, the problem of loose joint replacements can be a problem of bone loss, bone spurs, and damaged connective tissue. It can be much more than a hardware issue.
So now you can see why we see many patients with loose knee and hip implants. They are not in our office to get the hardware tightened or replaced, they are in our office to see if we can help them strengthen the connective tissue in the joint and create better stability, prevent wear and tear and the subsequent bone loss. If we can help these things, we diminish the body’s need to create bone spurs to stabilize the replacement joint. The formation of bone spurs and subsequent loss of range of motion is a primary cause of the need for a second joint replacement surgery.
In our office we offer regenerative medicine therapies using stem cells, growth factors, blood platelets in the form of Platelet Rich Plasma therapy, and Prolotherapy. These injections stimulate, repair and regrow the soft tissue of the joint including cartilage. The injections help prevent excessive motion and the wear and tear it causes. We also include hormone replacement therapy for some women because if hormones are lacking, it can make the healing more challenging.
What is the connection between low hormones and joint replacement problems? Inflammation
Examining the link between hormones and joint pain is something we obviously look at on a daily basis. When it comes to the degenerative problems of a joint replacement as we just mentioned above, we often find that the patient with chronic inflammation in the replacement joint. Inflammation is a multi-tool weapon. One of its tools is swelling. Swelling is a painful joint stabilizer, it prevents excessive motion in the joint. However to create swelling you must create inflammation. Inflammation in the short-term is the wound healing mechanism. Inflammation in the chronic long-term state is damaging and creates joint erosion. The goal of any treatment that seeks to prevent the need for a revision joint replacement surgery, is to shut down the chronic, corrosive, inflammation. Hormones replacement therapy may be an answer.
Stop the inflammatory destruction of bone with hormones.
Research lead by Oxford University showed hormone replacement therapy taken regularly for six months after a knee or hip replacement seemed to cut the risk for the need for repeat or surgery by around 40%.(1) How? By stopping bone loss with hormone replacement therapy.
The researchers wrote that osteolysis (the destruction of bone) and subsequent prosthesis loosening is the most common cause for revision following total knee replacement or total hip replacement. Hormone replacement therapy (HRT) could reduce osteolysis through its antiresorptive effects (The strengthening of bone using various factors, including estrogens).
Doctors at the University of Gothenburg, Sweden found that systemic inflammation not only destroys bone on its own, it also decreases estradiol levels in postmenopausal patients. The loss of estradiol further accelerating bone loss. (2)
In the journal Journal of biological regulators & homeostatic agents Italian researchers found that women do not do as well as men after joint replacement because of testosterone deficiency. Meaning that low testosterone can inhibit healing and repair.(3)
Recently doctors at the Mayo Clinic looked at the problem of 7 million people walking around with hip or knee replacements and the fact that the majority of these individuals will outlive their implants and require revision surgeries, mostly due to poor implant osseointegration (the bone and the implant did not fuses as well as hoped for) and aseptic loosening. Revision surgeries, they write, are potentially avoidable with better management of patient-related risk factors that affect the osseointegration of joint implants.
In their study the Mayo doctors focused on several systemic and local factors that are particularly relevant to implant osseointegration.
Examples include problems of hyperglycemia, oxidative stress, metabolic syndrome, high cholesterol and hormone hormone replacement therapy.(4)
Sometimes it is truly fascinating to see how the human body works and how seemingly unrelated fields of medicine are very related. For many people, problems of joint replacement implants is seen as a problem of hardware and mechanical stress. For others it is equally a problem that can be tackled with an holistic approach to healing.
If you would like to explore more information, please contact our office so we can start a conversation with you.
Related articles
Why Are Post-Menopausal Women Prone to Falls?
Why Are Post-Menopausal Women Prone to Falls?
References
1 . D. Prieto-Alhambra, M. K. Javaid, A. Judge, J. Maskell, C. Cooper, N. K. Arden, M. Mullee, J. Rafferty, A. Carr, A. Price, K. Javaid, D. Beard, D. Altman, N. Clarke. Hormone replacement therapy and mid-term implant survival following knee or hip arthroplasty for osteoarthritis: a population-based cohort study. Annals of the Rheumatic Diseases, 2014; DOI: 10.1136/annrheumdis-2013-
2 Andersson A, Bernardi AI, Nurkkala-Karlsson M, Stubelius A, Grahnemo L, Ohlsson C, Carlsten H, Islander U. Suppression of Experimental Arthritis and Associated Bone Loss by a Tissue-Selective Estrogen Complex. Endocrinology. 2016 Mar;157(3):1013-20. doi: 10.1210/en.2015-1820. Epub 2016 Jan 8.
3 Perego S, Grasso D, Bodini BD, Cavaiani F, De Santis C, Ursino N, Pelosi C, Banfi G, Lombardi G. Perisurgical and intra-rehabilitative salivary steroid hormone profiles in bicompartmental arthroplasty.J Biol Regul Homeost Agents. 2015 Oct-Dec;29(4):953-60.
4 Kremers HM, Lewallen EA, van Wijnen AJ, Lewallen DG. Clinical Factors, Disease Parameters, and Molecular Therapies Affecting Osseointegration of Orthopedic Implants. Current Molecular Biology Reports. 2016 Sep 1;2(3):123-32.




































Recent Comments