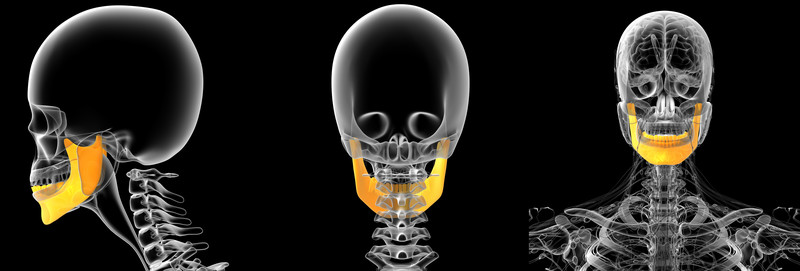
We see many cases of jaw or TMJ pain, facial pain, and headaches that have been unresponsive to traditional treatment measures such as painkillers, night guards, bite plates, or antibiotics for sinusitis. After an examination of the patients head, jaw and neck, we find that many of these patients can have their TMJ related pain traced to the occiput (the back of the skull), cervical facet joints, cervical interspinous ligaments, and the trapezium (trapezius) the muscle that extends from the back of the head to the thoracic region in the spine. If you have TMJ you will notice that we did not mention the mandible, the TMJ discs or the jaw in general. The reason for this is that if you are continuing to suffer with TMJ or TMJD (Temporomandibular Joint Disorder), the hunt for root cause of your symptoms must be expanded behind the jaw and the muscles of the jaw joint.
For someone who has bounced from one health care provider to another, be it dentist, physical therapist, chiropractor, and allied TMJ specialists, this hunt for TMJ symptom relief sometimes presents puzzlement in that the patient has been seeking treatments for years and a solid connection between problems in the cervical spine and their jaw pain had not been fully explored or even mentioned.
The idea of cervical neck problems causing TMJ problems for patients is not a new idea. This is something we have been exploring at the Magaziner Center for Wellness for many years. Research dating to 1998 showed that oral and maxillofacial surgeons in Belgium were seeing this problem in then increasing numbers:
They wrote of these findings in Clinical Oral Investigations. (1): Thirty-one consecutive patients with symptoms of TMJ indicated stability problems at the C0-C3 vertabrae levels and tender points in the trapezius and the large sternocleidomastoideus muscle.
In 2003, doctors in Japan found that the cervical spine impacted TMJ problems and TMJ problems impacted the cervical spine.(2) They found that in many TMJ patients the right and left masticatory muscles were in such a state of imbalance that they were causing the cervical spine to become displaced and this was greatly effecting these patient’s postures and bringing on a new myriad of symptoms that would eventually be traced back to the cervical spine.
In 2016, researchers built on these paper’s findings to determine if cervical neck motion exercises would relive jaw pain in patients with temporomandibular
The treatment of the cervical spine based on joint mobilizations, segmental stabilization, and muscle stretching produced statistically significant changes in subjects with TMJ.
The treatment protocol decreased self-reported pain, increased pain-free maximum mouth opening, and improved mandibular function. There was also a significant improvement in masticatory muscle sensitivity on the left side.
There was a statistically significant improvement in self-reported pain after intervention, with some subjects achieving a median of 0 on the pain scale.
TMJ muscles can make neck pain worse and neck muscles can make TMJ worse
All this now leads us to a study from November 2018 in the Canadian journal of physiology and pharmacology.(4)
In this study doctors questioned why the cervical neck muscles are not more full explored when treating patients with TMJ. The researchers note that disorders or impairments of the masticatory muscles (the “pain adaptation model” of TMJ) have an obvious effect on how the patient opens and closes their mouth to account for pain. They also note that “this model suffers several weaknesses; notably, it does not explain all types of neck muscle activities in neck pain, which is a very prevalent TMJ/TMD comorbid condition.” These researchers point out that the neck muscles may impact negatively on the TMJ muscles and cause further pain and a worsening degenerative condition. They conclude that there is a strong relationship between the neck muscles and the TMJ muscles, and, TMJ muscles can make neck pain worse and neck muscles can make TMJ worse.
TMD can make a woman’s headaches worse, headaches can make a woman’s TMD worse
At the Magaziner Center for Wellness, patients are evaluated by physical examination including but not limited to the strength of the arm and hands, integrity of the cranial nerves, sensory nerves and deep tendon reflexes, and range of motion of the neck. Furthermore, careful evaluation of the cervical facets, occiput, interspinous ligaments, and trapezium are performed by a physician skilled in diagnosis and treatment of such injuries. Injury in the latter regions, caused either by trauma, overuse, or degeneration is often responsible for causing headaches, jaw aches, and facial pain.
Cervicocranial syndrome (Barre-Lieou syndrome) can also occur from injury to the cervical facet joints. This syndrome is often manifest by a variety of findings such as vertigo, tinnitus, visual blurring, nasal stuffiness, and facial numbness.
Radiological studies such as plain radiographs and MRI may be useful in some cases of referred head, face, and jaw pain but often diagnose incidental findings that do not contribute to a patient’s pain syndrome. Findings such as degenerative disc disease, herniated cervical discs, or spinal arthritis may be incidental, as a significant percentage of the population (over 60% in some studies) demonstrate similar findings and remain asymptomatic.We strongly believe that a careful physical examination with clinical correlation is paramount to diagnosis and treatment of referred pain problems and can help to spare the patient from the cost and inconvenience of further diagnostic studies, treatments, and unnecessary medications for their TMJ and neck problems.
Treating TMJ pain with PRP Injections
PRP or Platelet Rich Plasma Therapy is derived from a patient’s own blood that consists of a combination of growth factors and platelets. When the body suffers a soft-tissue injury, its natural response is to deliver platelet cells to the area. Packed with growth and healing factors, platelets and other cells initiate repair and attract the critical assistance of stem cells. PRP therapy’s natural healing process intensifies the body’s efforts by delivering a higher concentration of platelets directly into an area of injury.
To create platelet-rich plasma therapy, a small sample of your blood is drawn, similar to a lab-test sample. The blood is placed in a centrifuge which separates the platelets from the other components. The concentrated platelet-rich plasma is then injected into and around the point of injury, jump-starting and significantly strengthening the body’s natural healing signal. Because the patient’s own blood is used, there is no risk of a transmissible infection and a very low risk of allergic reaction.
A 2020 study (5) published in the Journal of oral & facial pain and headache wrote: “Based on current evidence, PRP injections may reduce pain more effectively than placebo injections in TMJ osteoarthritis at 6 months (level of evidence: moderate) and 12 months (level of evidence: moderate) post-injection. This significant difference in pain reduction could also be seen when PRP was compared to hyaluronic acid at 12 months post-injection (level of evidence: low). It can be cautiously interpreted that PRP has a beneficial effect on the relief of TMJ osteoarthritis pain.
In September 2019 (6) a study suggested that treating patients with Disk displacement without reduction (misalignment causing joint pain and limited mouth opening) with PRP and arthrocentesis (fluid aspiration) appeared to be a superior treatment to arthrocentesis plus Hyaluronic acid injections or arthrocentesis alone.
In our clinical experience, initial improvement may be seen within a few weeks (depending on injury), gradually increasing as the healing progresses. Research studies and clinical practice have shown PRP therapy to be very effective at relieving pain and returning patients to their normal lives. Both ultrasound and MRI images have shown definitive tissue repair after PRP therapy, confirming the healing process. The need for surgery can also be greatly reduced by treating injured tissues before the damage progresses and the condition becomes irreversible.
If you would like to explore more information, please contact our office so we can start a conversation with you.
1. De Laat A, Meuleman H, Stevens A, Verbeke G. Correlation between cervical spine and temporomandibular disorders. Clinical oral investigations. 1998 Aug 1;2(2):54-7.
2. Shimazaki T, Motoyoshi M, Hosoi K, Namura S. The effect of occlusal alteration and masticatory imbalance on the cervical spine. The European Journal of Orthodontics. 2003 Oct 1;25(5):457-63
3. Calixtre LB, Grüninger BL, Haik MN, Alburquerque-Sendín F, Oliveira AB. Effects of cervical mobilization and exercise on pain, movement and function in subjects with temporomandibular disorders: a single group pre-post test. J Appl Oral Sci. 2016;24(3):188-97.
4 Fougeront N, Fleiter B. Temporomandibular disorder and comorbid neck pain: facts and hypotheses regarding pain-induced and rehabilitation-induced motor activity changes. Canadian journal of physiology and pharmacology. 2018 Aug 1;96(11):1051-9.
5 Li F, Wu C, Sun H, Zhou Q. Effect of Platelet-Rich Plasma Injections on Pain Reduction in Patients with Temporomandibular Joint Osteoarthrosis: A Meta-Analysis of Randomized Controlled Trials. J Oral Facial Pain Headache. 2020;34(2):149-156. doi:10.11607/ofph.2470
6 Toameh MH, Alkhouri I, Karman MA. Management of patients with disk displacement without reduction of the temporomandibular joint by arthrocentesis alone, plus hyaluronic acid or plus platelet-rich plasma. Dent Med Probl. 2019;56(3):265-272. doi:10.17219/dmp/109329




































Recent Comments