We are going to start with a 2011 study (1) and take a ten year trip through the research and bring ourselves current with the idea that estrogen can play a role in helping post menopausal women with chronic urinary tract infections and incontinence.
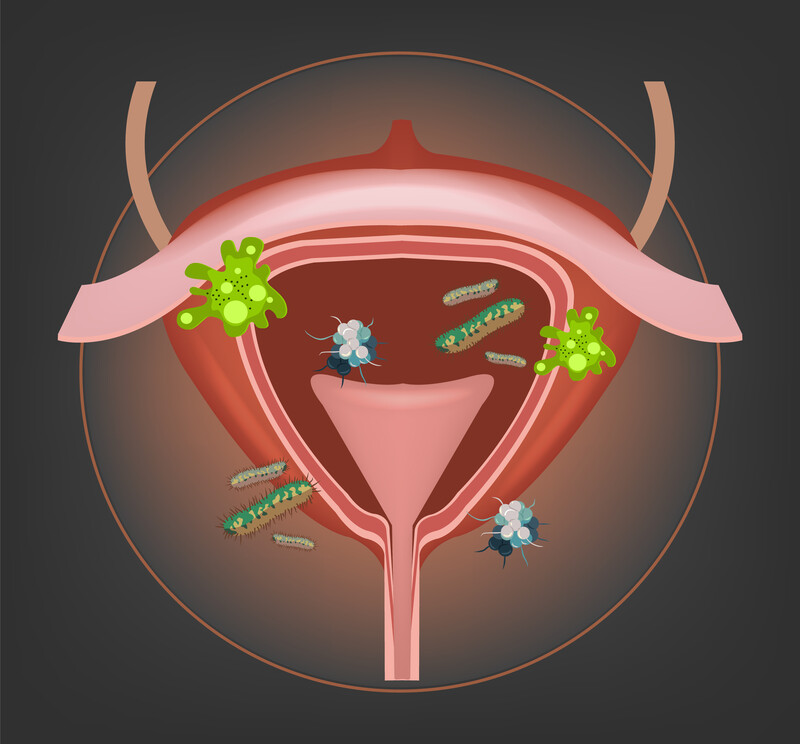
In this first study, researchers explored the potential role that estrogen deficiency plays in the development of bacteriuria or more plainly bacteria in the urine. Postmenopausal women frequently suffer from genitourinary symptoms; half have genitourinary disorders, and 29% have urinary incontinence.
Postmenopausal women of course can suffer from significant reduction in ovary estrogen secretion, which is often associated with vaginal atrophy. Clinically, it manifests as a syndrome characterized by vaginal dryness, itching, dyspareunia (vaginal pain), and urinary incontinence. This may sometimes imitate a urinary tract infection.
Estrogen stimulates the proliferation of lactobacillus in the vaginal tissue, reduces pH, and helps prevent vaginal colonization of Enterobacteriaceae, which are the main pathogens of the urinary tract.
A February 2021 in the medical journal Menopause (2) now offer us this:
“Genitourinary syndrome of menopause (GSM) refers to a collection of symptoms resulting from diminished hormonal, primarily estrogenic stimulation to the vulvovaginal or lower urinary tract and may affect up to 50% of postmenopausal women. Symptoms, which are typically progressive and unlikely to resolve spontaneously, may include, but are not limited to, vulvovaginal dryness, burning or irritation, dyspareunia, or urinary symptoms of urgency, dysuria or recurrent urinary tract infection.
These symptoms are typically progressive and unlikely to resolve spontaneously. Effective treatments include moisturizers and lubricants, local hormonal therapy with estrogen or dehydroepiandrosterone, and oral selective estrogen receptor agonists. . . Additionally, the influence and effect of the vaginal microbiome, as well as potential of treatment via its manipulation, is being studied.”
Vaginal Estrogen as First-Line Therapy?
In March 2021 doctors at the University of South Florida (3) examined how successful treatment with vaginal estrogen cream therapy could be for postmenopausal women with recurrent urinary tract infections and to identify risk factors for those who go on to require additional therapies beyond estrogen cream.
In this study, women had no prior history of treatment for recurrent urinary tract infections were started on vaginal estrogen cream alone as first-line therapy.
During the study period, 67.7% of 167 patients with recurrent urinary tract infections noted improvement or resolution in their symptoms with vaginal estrogen cream alone.
Women with a concomitant diagnosis of urinary incontinence, as defined as subjective report of bothersome stress or urgency urinary incontinence, were 2.3 times more likely to need additional therapy compared with women not reporting urinary incontinence.
It is usually more than just recurrent urinary tract infections
As the research above notes, urinary tract infections can be part of a more complex problem for post-menopausal women than estrogen cream can tackle. A previous paper reported observations (4) to this affect and that topically applied estrogen may help.
“Estrogen deficit in postmenopausal women causes urogenital atrophy, which is responsible for a wide range of urinary disorders (urinary incontinence, urge incontinence, recurrent urinary infections) and genital disorders (prolapse, dispareunya, vaginal dryness). The efficacy of estrogen therapy on urinary incontinence is not yet demonstrated, but it is widely recognized that the topical use of estrogens lowers the risk of recurrent urinary infections and improves urogenital atrophy.”
Going beyond cranberries to the gut microbiota
The suggestion to take cranberry extract to help with chronic urinary tract infections is well known and widely prescribed. Cranberry extract has been shown in many studies to be beneficial.(5) But some women have a greater challenge in managing their urinary disorders, more than cranberry extract may be able to help.
Another February 2021 study (6) made these comments on the role of cranberry extract and the importance of the beneficial bacteria of the gut microbiota.
“A recent placebo-controlled clinical trial found a 39% reduction in UTI symptoms among recurrent UTI sufferers who consumed a daily cranberry beverage for 24 weeks. Using metagenomic sequencing of stool from a subset of these trial participants, we assessed the impact of cranberry consumption on the gut microbiota, a reservoir for UTI-causing pathogens such as Escherichia coli, which causes more than 80% of UTIs.”
The researchers here are examining what role the cranberries had in altering the beneficial bacteria of the gut microbiota. What they found was that the cranberries, while helping with the UTIs, did not positively impact or significantly change the bacterial composition of the gut microbiota.
More than just urinary tract infections and overactive bladder
In many patients we see, overactive bladder is not the primary complaint of their health concerns. It is a problem within many problems and in many cases a symptom of a greater problem. That problem is metabolic syndrome. Metabolic syndrome is a constellation of developing health problems that include type 2 diabetes, high blood pressure, high cholesterol, and being overweight and obese. It is often suggested to doctors that in their initial consultation with a patient, that a large waist line or big belly should be a clear indication that Metabolic Syndrome is present in this patient.
If you would like to explore more information, please contact our office so we can start a conversation with you.
Related articles:
Older Men and Women Not Getting Good Information From Doctors on Overactive Bladder
1 Raz R. Urinary tract infection in postmenopausal women. Korean journal of urology. 2011 Dec 1;52(12):801-8.
2 Phillips NA, Bachmann GA. Genitourinary syndrome of menopause and age: a new algorithm for hormonal treatment?. Menopause. 2021 Feb 1;28(2):109-10.
3 Chang E, Kent L, Prieto I, Eggers E, Tanner JP, Bassaly R, Wyman A, Greene K. Vaginal Estrogen as First-Line Therapy for Recurrent Urinary Tract Infections in Postmenopausal Women and Risk Factors for Needing Additional Therapy. Female Pelvic Medicine & Reconstructive Surgery. 2021 Mar 1;27(3):e487-92.
4 Della Martina M, Xodo S, Vogrig E, Rinuncini D, Ganzitti L, Driul L, Fabiani G, Marchesoni D. Hormone replacement therapy and urogenital disease in postmenopausal women. Minerva Ginecol. 2012 Aug;64(4):337-44.
5. Burleigh AE, Benck SM, McAchran SE, Reed JD, Krueger CG, Hopkins WJ. Consumption of sweetened, dried cranberries may reduce urinary tract infection incidence in susceptible women – a modified observational study. Nutr J. 2013 Oct 18;12(1):139. doi: 10.1186/1475-2891-12-139.
6 Phillips NA, Bachmann GA. Genitourinary syndrome of menopause and age: a new algorithm for hormonal treatment?. Menopause. 2021 Feb 1;28(2):109-10.
































Recent Comments