Sleep problems are common in people who have symptomatic Alzheimer’s disease, but scientists are suspecting that they also may be an indicator of early disease. This medical suspecion has been investigated for many years and answers are still not that clear. A 2013 paper suggested that participants who had preclinical Alzheimer’s disease had poorer sleep efficiency (80.4 percent) than people without markers of Alzheimer’s (83.7 percent). On average, those with preclinical disease were in bed as long as other participants, but they spent less time asleep. They also napped more often.(1)
Sleep concerns among aging adults are very common. Typically people will try to manage this on their own with sleep aids, over-the-counter sleep medications, or other advice they researched. In our office we see many people with more advanced symptoms and this will require more advance treatment protocols. As this article is about Sleep and Alzheimer’s disease, let’s look at three new studies that discuss the connection with sleep problems and the early onset of Alzheimer’s disease.
July 2021 in The Journal of neuroscience.(2)
Sleep disturbance can be seen as predictive of Alzheimer’s Disease
Alzheimer’s disease is associated with sleep disruption, often before significant memory decline. Thus real-life patterns of sleep behavior have the potential to serve as a window into early disease progression. . . The researchers examined 89 cognitive healthy older adults and found that tau burden was associated with worse wristwatch actigraphy-measured sleep quality (a sleep measurement watch), and that both tau and β-amyloid (proteins associated Alzheimer’s disease) with were independently predictive of self-reported sleep quality.
Furthermore, individuals with greater β-amyloid deposition were more likely to underestimate their sleep quality, and sleep quality underestimation was associated with worse executive function. These data support the role of sleep impairment as a key marker of early Alzheimer’s disease, and offer the possibility that actigraphy (sleep wrist watch) may be an affordable and scalable tool in quantifying Alzheimer’s-related behavioral changes.
Sleep and wake disorders are often misdiagnosed and undertreated in typical Alzheimer’s disease
March 2021 in the journal Alzheimer’s & dementia.(3)
“Although, the clinical variants of Alzheimer’s disease (AD) show distinct patterns of cognitive and behavioral decline, disease progression, and neuropathological features, it is unclear if this clinical heterogeneity extends to sleep-wake patterns. Sleep and wake disturbances are frequent in typical Alzheimer’s disease, often preceding memory loss and negatively impacting the quality of life of patients and caregivers alike. Still, sleep and wake disorders are often misdiagnosed and undertreated in typical Alzheimer’s disease.
Better characterization of sleep-wake features in Alzheimer’s disease clinical variants is an unmet gap of high importance because these differing patterns (varying levels of sleep disturbance in Alzheimer’s patients) may require tailored treatment strategies. Moreover, as wake-promoting neurons (the cells that make you wake up) are located in subcortical nuclei and degenerate early in typical Alzheimer’s disease, contrasting the profiles of sleep-wake patterns in typical and atypical Alzheimer’s disease aids diagnosis and brings a unique opportunity to uncover the mechanisms underlying Alzheimer’s disease clinical variants. . . “
What is being suggested is that sleep disturbance occurs in different ways in the aging population and that these differences should be recognized and treatment tailored to the individual.
Circadian rhythm disruption may contribute to the development and progression of the neuropathological changes occurring in Alzheimer’s disease
January 2020 in The European journal of neuroscience.(4)
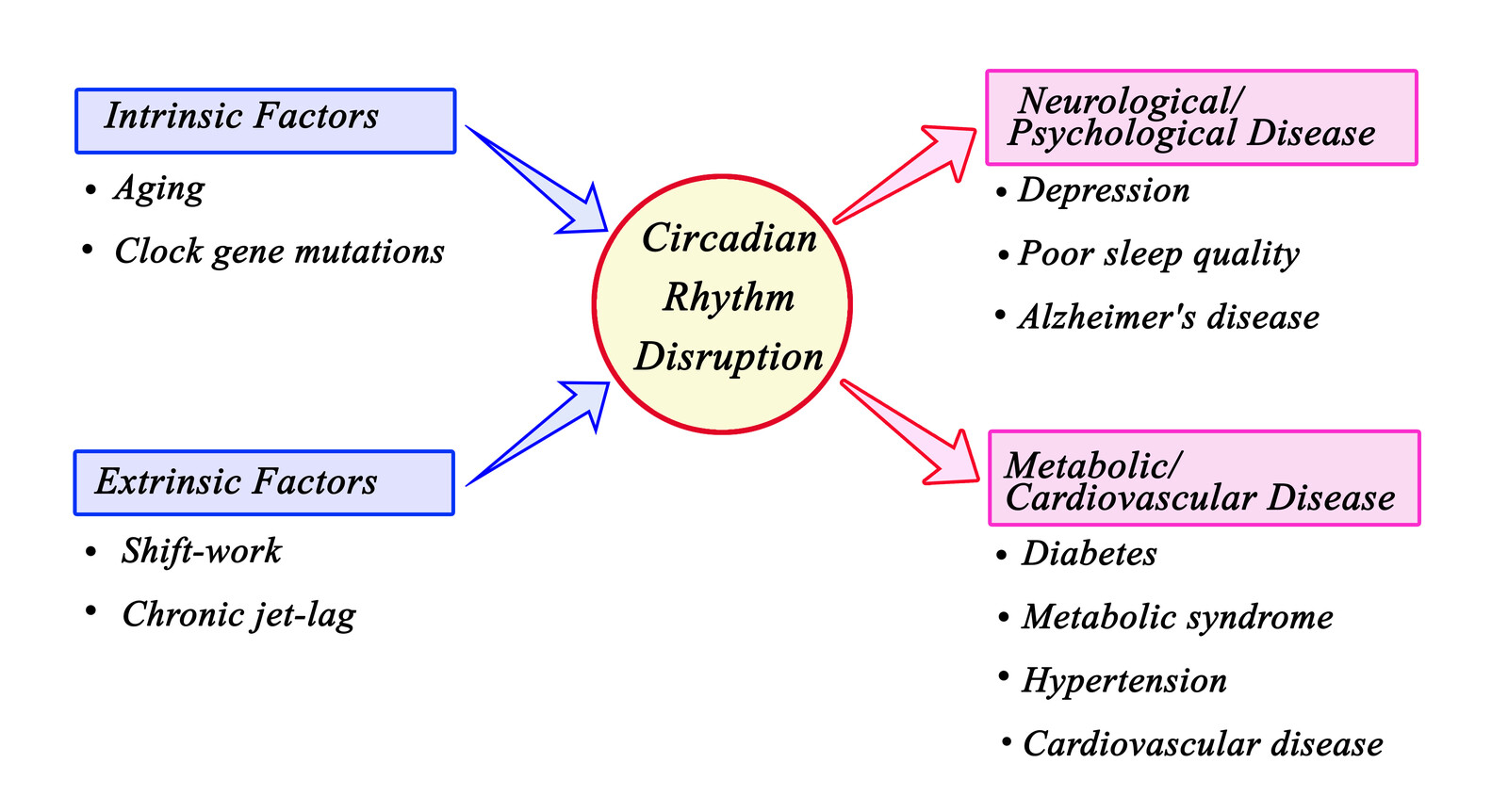
Aging leads to changes in circadian rhythms (the natural sleep-wake cycle or clock), including decreased amplitude or robustness (in other words your internal clock which usually keeps good time, especially when you are younger, starts to “lose time” or not measure time that well as you age), altered synchrony with the environment (sleep during the day, wide awake at night to the point of being restless), and reduced coordination of rhythms within body.
These circadian rhythm alterations are more pronounced in age-associated neurodegenerative disorders such as Alzheimer’s disease, in which they often precede the onset of other symptoms by many years. As well as their early onset, the findings that fragmentation of daily rest-activity rhythms in non-demented older subjects is associated earlier cognitive decline, increased risk of incident Alzheimer’s disease, and preclinical Alzheimer’s disease neuropathology, suggest that circadian rhythm disruption may contribute to the development and progression of the neuropathological changes occurring in Alzheimer’s disease. Conversely, other studies have implicated amyloid-beta, a prominent neurotoxin that accumulates in Alzheimer’s disease, in the impairment of circadian rhythms.
The suggestion is that altered sleep cycles may increase risk of Alzheimer’s disease and it may be a preventable condition.
This is the subject of a July 2021 study in the Journal of the American Medical Association (JAMA) (5). It will help tie everything together.
The researchers write: “Disrupted sleep commonly occurs with progressing neurodegenerative disease. Large, well-characterized neuroimaging studies of cognitively unimpaired adults are warranted to clarify the magnitude and onset of the association between sleep and emerging β-amyloid (Aβ) pathology (the protein buildup in the brain that is seen as a cause of Alzheimer’s Disease).”
What the study sought to identify was the association between daytime and nighttime sleep duration with regional Aβ pathology (only impacting certain regions of the brain) in older cognitively unimpaired adults.What they found was an increased risk of Aβ deposition with reduced nighttime sleep duration occurred early before cognitive impairment or significant Aβ deposition. Daytime sleep may be associated with an increase in risk for early Aβ accumulation and did not appear to be corrective for loss of nighttime sleep, demonstrating a circadian rhythm dependence of sleep in preventing Aβ accumulation. Treatments that improve sleep may reduce early Aβ accumulation and aid in delaying the onset of cognitive dysfunction associated with early Alzheimer disease.
Sleep is one component of good health. At the Magaziner Center, we strive to address the root causes of health issues that have not responded to conventional treatments, utilizing the latest testing techniques to do a thorough assessment of your body’s unique biochemistry. We help restore your body to optimal health by taking into account dietary habits, emotional and environmental factors, lifestyle and a good deal more. Remember, your body has been endowed with the ability to heal itself. What we do is to provide it with supportive natural and holistic therapies designed to help make that happen.
If you would like to explore more information, please contact our office so we can start a conversation with you.
Similar articles
Research on Vitamin B12 and Folic Acid Deficiency Connected to Alzheimer’s Disease and Dementia
Post-Menopausal Memory Loss
References
1 Ju YE, McLeland JS, Toedebusch CD, Xiong C, Fagan AM, Duntley SP, Morris JC, Holtzman DM. Sleep quality and preclinical Alzheimer disease. JAMA neurology. 2013 May 1;70(5):587-93.
2 Winer JR, Morehouse A, Fenton L, et al. Tau and β-amyloid burden predict actigraphy-measured and self-reported impairment and misperception of human sleep [published online ahead of print, 2021 Jul 21]. J Neurosci. 2021;JN-RM-0353-21. doi:10.1523/JNEUROSCI.0353-21.2021
3 Falgàs N, Walsh CM, Neylan TC, Grinberg LT. Deepen into sleep and wake patterns across Alzheimer’s disease phenotypes. Alzheimer’s & Dementia. 2021 Mar 12.
4 Duncan MJ. Interacting influences of aging and Alzheimer’s disease on circadian rhythms. European Journal of Neuroscience. 2020 Jan;51(1):310-25.
5 Insel PS, Mohlenhoff BS, Neylan TC, Krystal AD, Mackin RS. Association of Sleep and β-Amyloid Pathology Among Older Cognitively Unimpaired Adults. JAMA Netw Open. 2021;4(7):e2117573. Published 2021 Jul 1. doi:10.1001/jamanetworkopen.2021.17573




































Recent Comments